Can I describe my experience from the beginning, in excruciating detail? Is it at all necessary or helpful? Prior to my surgery I read a lot of really technical journal articles I didn’t understand, scrolled endlessly through oddly-colored diagrams illustrating the surgery process (the human body is just a bunch of goddamn flaps!), and read multiple message board posts by other women looking for reassurance. I did not find any of it particularly helpful (also, can we talk about the number of “lady mag” articles out there pushing the narrative of going back to work and running marathons as soon as possible? It doesn’t empower, it only serves to shame); what I really wanted was someone to detail their surgery experience from start to finish.
I think part of the reason those stories are so hard to find is that your brain tries to cover up the trauma. I can sit down and run through the day of surgery in my mind— my body remembers every moment in the hospital— but when I open my mouth to try and explain it words fail me.
Our call time was 5:30, which meant we had to get up at 3 in order to do one last hibiclens shower (sort of like showering in unpleasant, dry slime) and drink clear Ensure. I was actually grateful for the Ensure, since I am a breakfast person and the combination of being NPO and nerves usually yields some next-level nausea. This surgery was at a different hospital than our usual (the fact that we even have a usual hospital is deeply irritating), and the pre-op process felt foreign. Hospital decor is always lacking, but this hospital was especially bad— whoever decided on floor-to-ceiling paper bag brown should be arrested. Old hospitals seem to believe that natural light keeps you sick, and do all they can to keep you from ever catching a glimpse of the sky again.
Pre-op is hard. There is a moment when you change from your street clothes to your hideous gown, and you feel like you’re shedding your human skin to become something less than. I always try to counter that feeling by showing up with elaborate nails, but I was not allowed to have fingernail polish for this surgery— my plastic surgeon wanted to ensure we were getting a 100% accurate read on my oxygen, and I was obviously in no position to argue. I was upset at first, but reoriented and got a rainbow pedicure reading “Fuck Cancer”, which I accompanied with bright pink socks printed with middle fingers. Anything you can do to make yourself feel more like yourself and less like a giant depersonalized bag of flesh is vital— and it also helps provide fodder for conversation at a time where pulling out words can feel like a ridiculous ask.
I was most afraid of how I would handle my plastic surgeon making guide marks on me before surgery. I’d seen countless photos on instagram of women laughing their way through it, crying, or just ignoring it— every time I tried to envision it, I saw myself turning into dust. For weeks, it was the most anxiety provoking part for me; here’s this part of my body a relative stranger is going to come in and draw on, so she can know where to cut it off. As someone who has struggled with dissociating and even just figuring out where my body exists in space, this was too much for my brain to handle. That’s where valium comes in! My breast surgeon knows me well, and had already written a prescription so I was feeling remarkably free and easy.
Mastectomy and reconstruction sometimes feels like a series of indignities strung together into one long, confusing nightmare. One special little pre-surgery indignity is the four shots you get in your nipple so they can see which lymph nodes to biopsy once they get in there— I still haven’t quite shaken the feeling that its pretty unfair that the last thing my poor nipple felt was four shots, but the pain was minimal and what are you gonna do? Aaron went with me as they wheeled me back to nuclear medicine, and I took my first opportunity (of what would be many) to force hospital employees to watch my stellar Icelandic puffin footage. My sister teased me for showing so many people, but every time I made someone watch it gave me thirty seconds of existing outside the hospital bed.
Pre-op is strange, especially for a major surgery like this. People want to be there to wish you well, to hug your neck and tell you you’re brave…but I sometimes can’t shake the dark thought that everyone wants to see you one last time in case you die. My room was crowded, but my mom and sister in particular are experts at keeping things light and laughing at the heaviness. There is a blank spot in my memory— I remember everyone being in the room and I remember being wheeled back to the OR, but I can feel a tearful gap in between. I know Aaron and I had a moment alone, but everything happened very quickly. I can remember being wheeled into the OR for every surgery I’ve had; I feel the rush of cold immediately beyond the double doors, I see the surgical lights that remind me of a confused octopus, a shiny jumble of ominous looking equipment, and what feels like a million clocks on the wall. I feel an urge to be chatty right before I go under, as if to remind myself and the OR staff I am human.
Waking up from surgery is like falling out of a watercolor; my initial memories are hazy swirls of color (brown, brown, and more brown mostly) that eventually harden into objects. I remember a voice telling me “you didn’t use your pain pump once!” so I must have been awake in the recovery room, but the first concrete thing I remember is being wheeled into my room and Aaron appearing and showing me how he’d taught himself to floss during the eleven hours I was in surgery. The flossing enraged and confused me— I didn’t understand how or why a human body was moving so quickly, but I think all I managed was a blank stare. According to Aaron, the flossing actually took place a couple days later so I guess this is a testament both to my confusion and the power of the floss.
Going in, I knew the room would be kept warm after surgery but I didn’t realize that meant I was going to be kept under what was essentially a heated pool float and be sporting a full oxygen mask. I’m sure this was included in the deluge of information I received leading up to surgery, but I had assiduously avoided most everything and transferred all responsibilities to poor, dutiful Aaron. I tend to run hot, so I was deeply unhappy to be under that blanket and my nurse very kindly let me poke my feet out at the end to try and cool off.
Waking up with an oxygen mask was not my favorite. Its traumatic in and of itself, compounded by the fact it really reminded me of my dad’s final few days in the hospital. I learned to appreciate it, though, since the forced air helped keep my sweat cool and basically acted like the world’s saddest, most expensive personal A/C. My mom was my hero and bought a little USB fan that attaches to your phone, and she and Aaron took turns fanning me so I didn’t have a complete and total breakdown.
I know I packed a bag for the hospital the night before, but I have no idea what I packed (this happened a lot in the lead up to surgery— I was supposed to take a trip to Denver and at one point I’d packed three shirts, eight pairs of underwear, and no pants). I had envisioned myself in my hospital bed, wearing ugly Old Navy button downs I’d embroidered with “fuck cancer”, reading books, and watching movies when I couldn’t sleep. I’d picked up a rock in Iceland to serve as a worry stone, had hand lotion I bought at the Blue Lagoon specifically for reminding myself I was a human who took trips in the moments when I felt like a growth attached to a hospital bed, and a wide array of essential oils to sniff like a deranged Sherlock Holmes when I got caught up in a trauma response. Instead, this is what happened: I focused 100% on just existing. Surgery compressed my personality into paper— flat and dull. At one point Aaron tried playing Bob Ross to help me fall asleep, but his gentle whisper made me rage.
I remember how my shoulder hurt; eleven hours in a crucifixion pose will do that to you, and I already carry my stress in my left shoulder. It is an odd feeling to wake up and be unable to move— I remember saying I wanted to pop my shoulder, but knowing better and focusing on small range of motion exercises for my wrists. I might’ve tried to text, but texting was an inaccessible joke and concentrating made me feel like I was disappearing. My breasts were swaddled in gauze and compressed within a pink surgical bra. I don’t remember feeling pain, in particular, just discomfort and a lot of tenderness at my drain sites. My abdominal incision, though, was a lot to handle.
They warn you ahead of time your incision will run hip to hip, but you don’t really process that until you have it. All of the sutures are internal, so when you wake up you are greeted by what seems like an open wound, a jagged Joker smile covered by yellow strip of cloth covered in bacitracin. This strip is changed regularly, and every touch is a kind of pain I find hard to describe. Its so painful its almost not— its like your nerves light up with a pain so sharp it feels sickly sweet, and then your brain refuses to process any more.
I woke up with six drains, the tubes twisting around each other like ribbons. I’d had a drain only once before, in my neck after thyroid surgery (even though that drain was tiny, in many ways it bothered me more than these six— the neck is a weird, fragile place). I had two drains beside either breast, and a drain in each hip. Dealing with them was not that bad when I still had a catheter, since my only job was to be still. The nurses would strip my drains, which involved pinching and then running your fingers down the tube to move the fluid into the drain. I got used to the ghastly sucking noise the drains made every time they were emptied into the measurement cups, but I always felt a dull, uncomfortable tugging. Those suckers are deeper in than you’d think, and your body is not thrilled about having a foreign object hanging around.
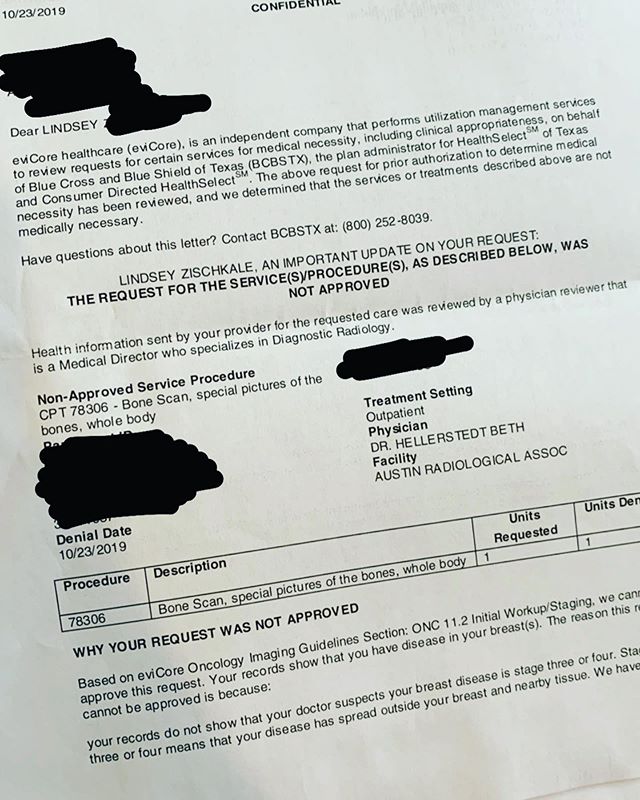
My nurses were amazing, and I fell into the rhythm of the hospital. Grab handfuls of sleep when you can, order food as if you intend to eat it, get your pain medicine, watch the doctor, nurse or PA check your flaps, repeat. Usually each flap is monitored by an oxygen sensor— your reconstructed breasts need to stay above a certain oxygen percentage to make sure they “take”, and the readings are pushed the the surgeon’s phone. My left breast was not cooperative, continually giving low or funky readings; there was a scary moment where my room was full— two nurses, my surgeon, the PA, my mom, my sister, and my husband. My surgeon can lay down the law when she needs to (see: putting the fear of god in me to eat real food and not just Ensure), and this was one of those moments. The tissue on my left breast did not believe in allowing a good reading, so they switched to using a doppler to listen for the sound of the artery. Every hour on the hour for the next five days, a nurse, PA, or my surgeon would come in, run the doppler over my left breast in search of the vein, and there would be a breathless moment where I could not hear anything and I wondered whether this would be the time I lost the flap.
Blessedly, this never happened. No matter the delay, eventually I would hear the wet, whooshing noise of the blood rushing through the vein, and for the next 55 minutes I would be relieved. I would occupy the time until the next check by trying to eat hospital food (I ordered beef medallions almost every day, and struggled to eat them almost every day), closing my eyes in a sad attempt to sleep, and at one point watching the Mueller testimony.
This is already overly long, so I will save the fun things— catheter removal, how walking three feet to a chair can feel like 26 miles, and the ugly magic of your first shower post-DIEP— for part two.